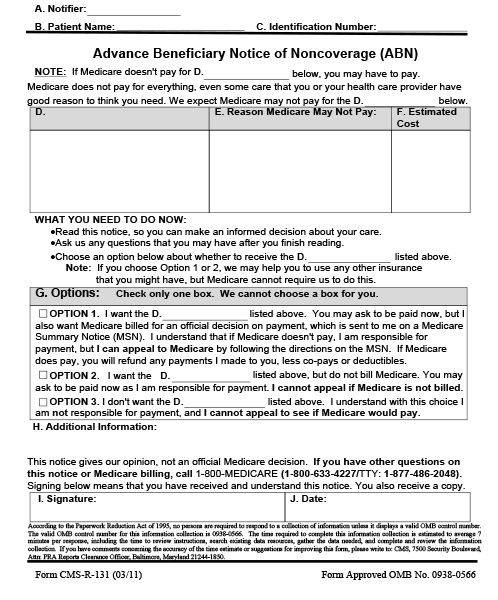
This is how the Advance Beneficiary Notice of Noncoverage works, if you have Original Medicare and any provider or supplier thinks that Medicare probably (or certainly) won’t pay for items or services because Medicare deems the treatment not medically necessary, that provider or supplier is required to provide you with a written notice called an “Advance Beneficiary Notice of Noncoverage” (ABN). There are exceptions, an ABN isn’t required for items or services that Medicare never covers.
The ABN lists the items or services that Medicare isn’t expected to pay for, an estimate of the costs for the items and services, and the reasons why Medicare may not pay. The ABN gives you information to make an informed choice about whether or not you wish to get items or services, understanding that you may have to accept responsibility for payment. However, on the rare occasion a provider or supplier fails to give you an ABN and Medicare declines coverage, that provider or supplier cannot bill you for any unpaid services or supplies that Medicare did not cover.
When completing an ABN, you’ll be asked to choose an option box and sign the notice to say that you read and understood it. You must choose one of these options:
- Option 1: You want the items or services that may not be paid for by Medicare. Your provider or supplier may ask you to pay up-front, but you also want them to submit a claim to Medicare for the items or services. If Medicare denies payment, you’re responsible for paying, however, because a claim was submitted, you can appeal to Medicare.
- Option 2: You want the items or services that may not be paid for by Medicare, and you don’t want your provider or supplier to bill Medicare. You may be asked to pay for the items or services up-front, and because you request your provider or supplier to not submit a claim to Medicare, you can’t file an appeal.
- Option 3: You don’t want the items or services that may not be paid for by Medicare, and you won’t be responsible for any payments as no item or service was provided. A claim isn’t submitted to Medicare, and no appeal can be filed to Medicare.
An ABN isn’t an official denial of coverage by Medicare. You have the right to file an appeal if payment is denied when a claim is submitted.